Why "Fatty Liver" is Now an Important Condition to Pay Attention to
If you are diagnosed with a "fatty liver", there are now ways to reverse it.
The Book - Kindle Version Now Available Worldwide
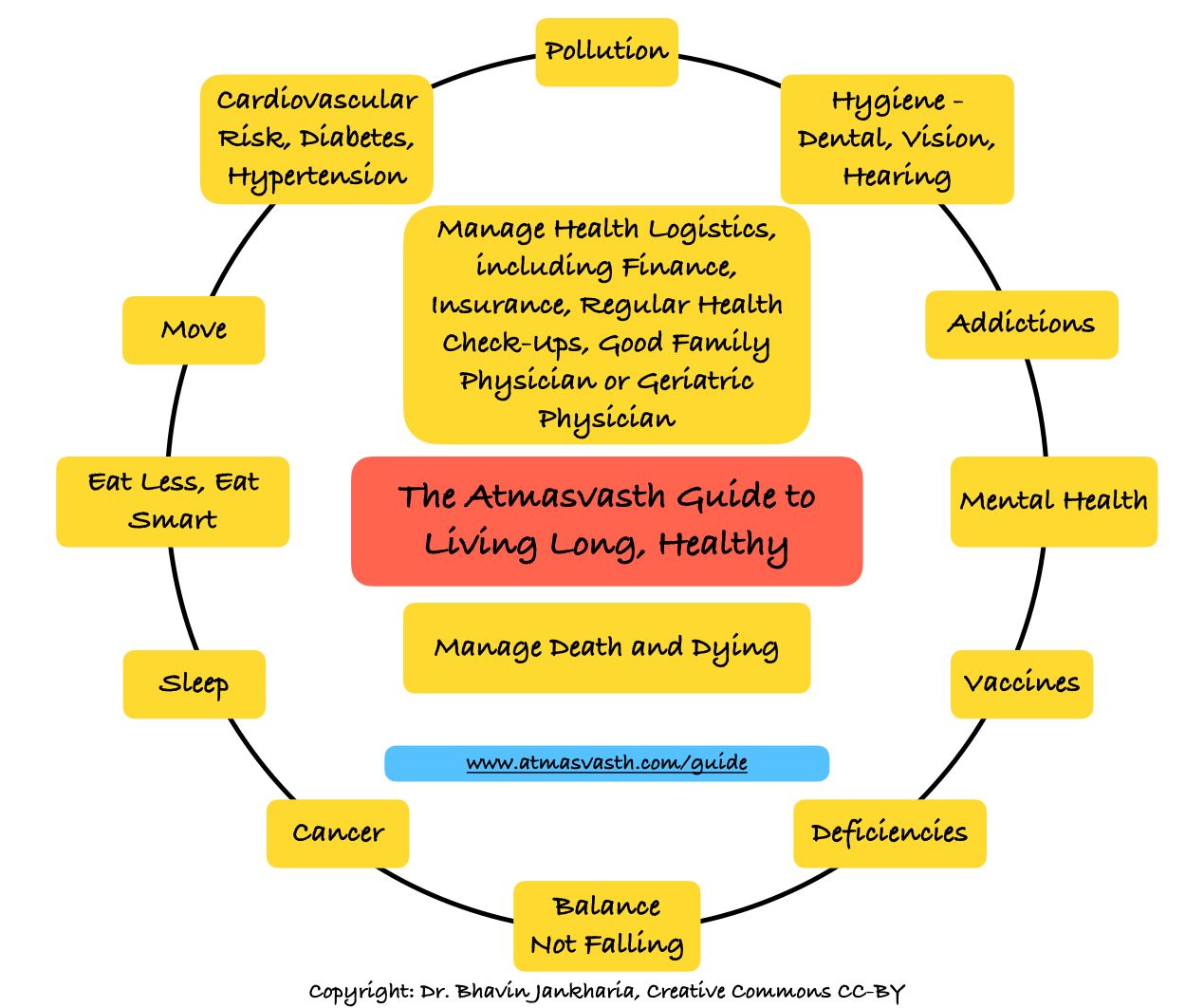
The Detailed 15-Point Guide to Live Long, Healthy
Audio
Soundcloud
YouTube
A YouTube version of the audio is also now available here.
Text
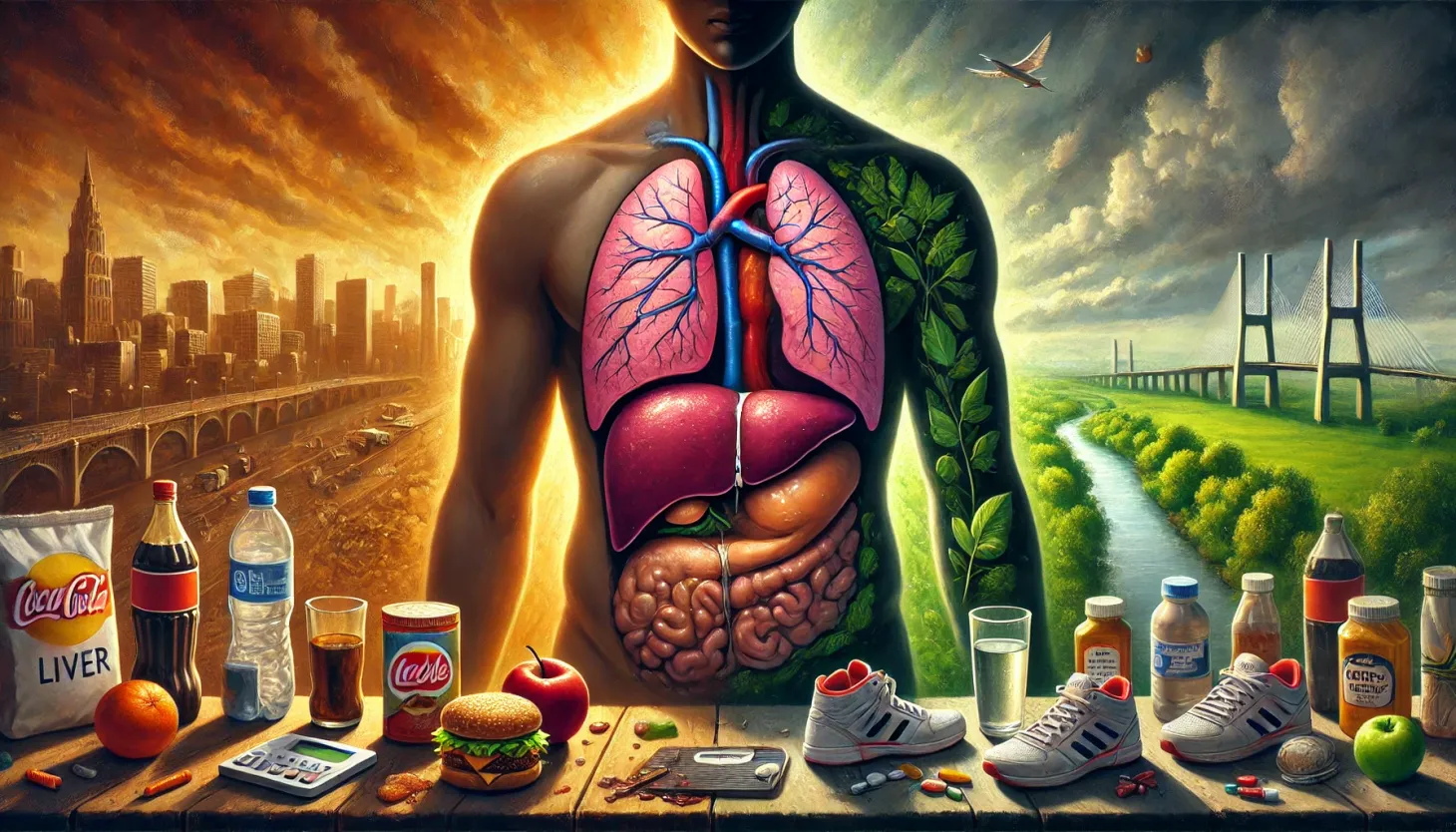
A good number of people have a “fatty liver”, which is a lay or popular term for hepatic steatosis, which affects a large number of people (up to 30% in the Western world).
Steatosis can be due to alcohol consumption, but is increasingly being seen in people who don’t consume alcohol. The typical reasons are other risk factors such as obesity, diabetes, sedentary lifestyle, etc.
Why is this important?
The prevalence is high in India, ranging from 28.1% in average-risk groups to 52.8% in high-risk groups, for an average prevalence of 38.6% [1]. This means that 1/3rd of India’s adult population has a “fatty liver”, which is concerning, since this is the kind of prevalence we associate with diabetes and high blood pressure (and diabetes itself is a risk factor for hepatic steatosis).
The reason this is relevant is because a certain number of patients (20-25%) with steatosis will progress to inflammation (steatohepatitis), of whom, a certain number (20-25%) will progress to liver fibrosis and early death. Even though liver transplant is increasingly a solution for treating end-stage liver disease, it is still a drastic solution that curtails lifespan.
So how do you know if and when you have a “fatty liver”?
You may get a diagnosis of “fatty liver” even if you have no symptoms, typically when you go for ultrasound of the abdomen for some other reason or when you go for an annual health check-up, especially one of those fancy ones where unnecessary tests are done for no reason. Sometimes this may be picked up on CT scans of the chest or abdomen.
There is currently no guideline or rationale for screening for hepatic steatosis in the general population, unless you have specific risk factors and your doctor believes you are at high risk and need to be checked for steatosis. A popular test for steatosis is a fibroscan, which is an ultrasound based test and can tell you not only if you have steatosis, but also if you have liver fibrosis.
So what do you do if you are labeled to have a “fatty liver”?
The challenge with a diagnosis of steatosis and you may hear terms like NASH, NAFLD, MASH, MASLD, MetALD, etc, is that there has been on definitive treatment for this condition until very recently. Which means, even if you were diagnosed to have steatosis, the best that could be done to reverse it would be alcohol abstinence or reduction, change in diet, increased physical activity, control of diabetes, high blood pressure and weight reduction, all interventions that are anyway done as part of a healthy lifestyle. The results of these interventions have also been very iffy.
Early last year, one drug, resmetirom [2], was finally approved for use in hepatic steatosis. But this is a new class of drugs, not currently available in India as of May 2025, and expensive (currently Rs. 15,000 odd per 100 mg tablet per day).
And then this 30th April, everything changed.
The NEJM [3] published an exceptionally well-conducted study on patients with hepatic steatosis and fibrosis, where semaglutide, a GLP-1 agonist was used in a randomized manner. The results are excellent with a significant number of people showing reversal of steatosis and fibrosis both, proven on liver biopsy.
This is a game-changer, because semaglutide and other GLP-1 agonists are increasingly available in India for diabetes control, but more importantly for weight control, whether obese or normal weight. For many people, GLP-1 agonists are a way to look good and many celebrities have been using them for some time now (if you see an actor/actress who is suddenly looking trim but with the face a little indrawn, you know they are on one of these drugs).
In the coming years, unless some unknown major complication/side-effect crops up over long-term use, GLP-1 agonists will be commonly used like aspirin, statins, anti-blood pressure and other anti-diabetic drugs, cheap and easily available. Even though, the NEJM study was done with injectable semaglutide, eventually oral versions of these drugs will commonly be used - currently a single table of Rybelsus 14 mg costs Rs. 348 per day, which is affordable and can be considered for use over a longer period of time (it comes to around Rs. 10,000 per month). The injectable versions of semaglutide and tirzepatide cost more but are still in the range of Rs. 3500 per week, so around Rs. 14,000 per month.
If a drug that is easily available and has few side-effects currently can reverse hepatic steatosis and hence potentially prevent fibrosis and cirrhosis and reduce the need for liver transplants, then it makes sense to screen and diagnose hepatic steatosis early. Even though guidelines do not support screening in the general population, you should ask the doctor to check for a “fatty liver” anytime you are getting a sonogram or a CT scan or an MRI of the chest or abdomen.
What does this mean for you and I?
If you find yourself with a diagnosis of “fatty liver” or “liver or hepatic steatosis”, you should have a conversation with your physician about how to reverse this. While lifestyle interventions will be first on the list, using semaglutide, tirzepatide or other GLP-1 agonists may be worth the effort and should be discussed in that conversation.
My understanding is that in the future when these drugs are sold without prescription or when prescriptions for these drugs are easily available, as with statins, people will just take GLP-1 agonists on a routine basis, which will automatically reduce the burden, not just of overweight/obesity and diabetes but also of “fatty liver” and its consequent long-term liver problems.
I will discuss the increasing use of GLP-1 agonists for anything and everything as if they are that one-wonder drug we have all been waiting for, in a post in the near future, especially its use to control weight, even if you are not overweight or diabetic.
Footnotes
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.
