The Relevance of Visceral Adiposity and Android Fat
Levels of physical inactivity and BMI measured obesity are rising in Indians, especially in those over age 50. Visceral adiposity is a more important measure and should be understood, measured and then addressed.

The Book
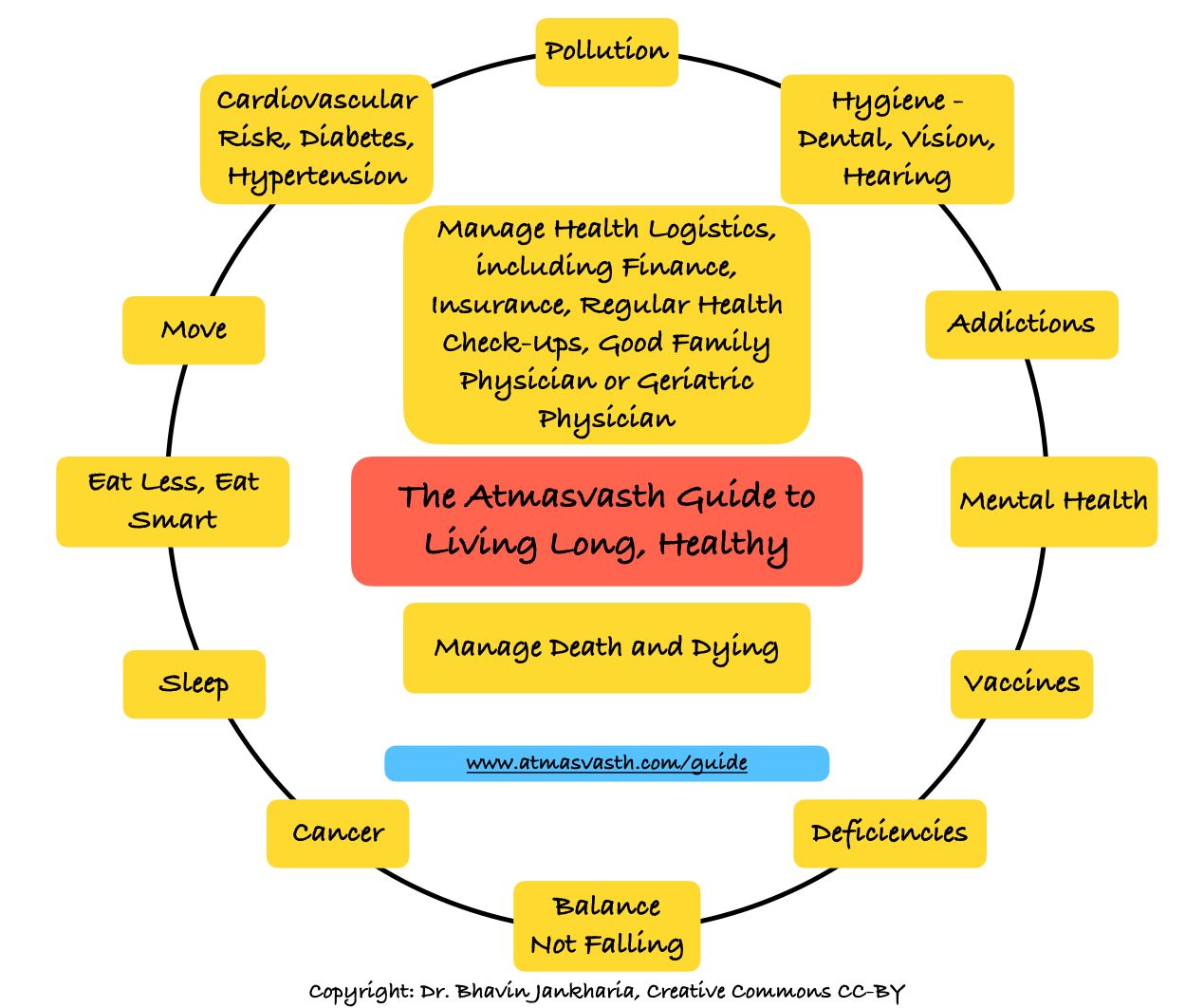
The Detailed 15-Point Guide to Live Long, Healthy
Audio
Soundcloud
YouTube
A YouTube version of the audio is also now available here.
Text
My fundamental take on so-called obesity has always been that outside of morbid obesity (BMI>35 kg/sq m), it is better to be overnourished than undernourished and more importantly, it is better to be fit and overweight than normal weight and unfit.
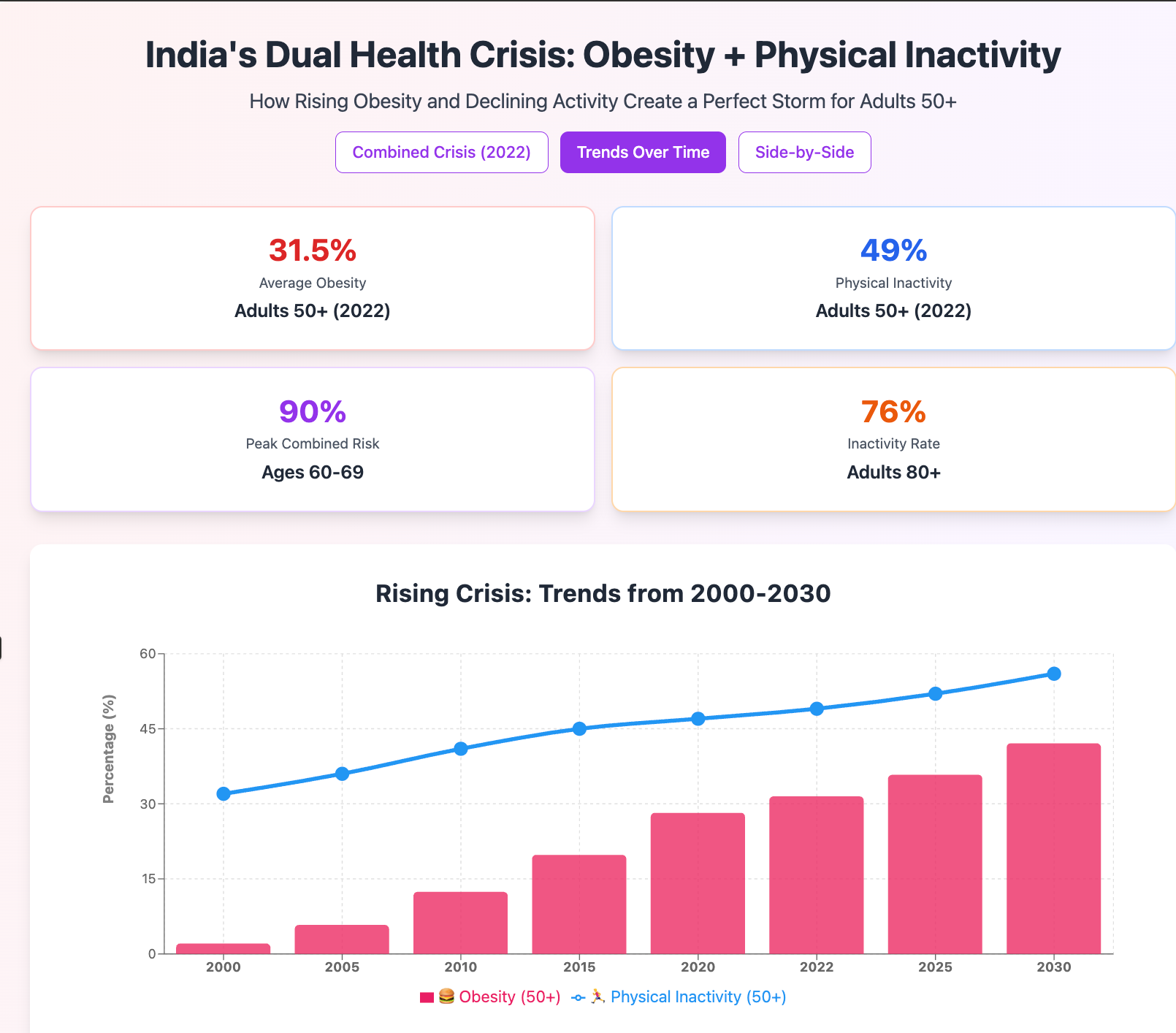
The challenge however is that more than half the Indian population over the age of 50 is unfit as seen in this graph based on the data from the “insufficient physical activity among adults from 2000 to 2022” paper using WHO data [1].
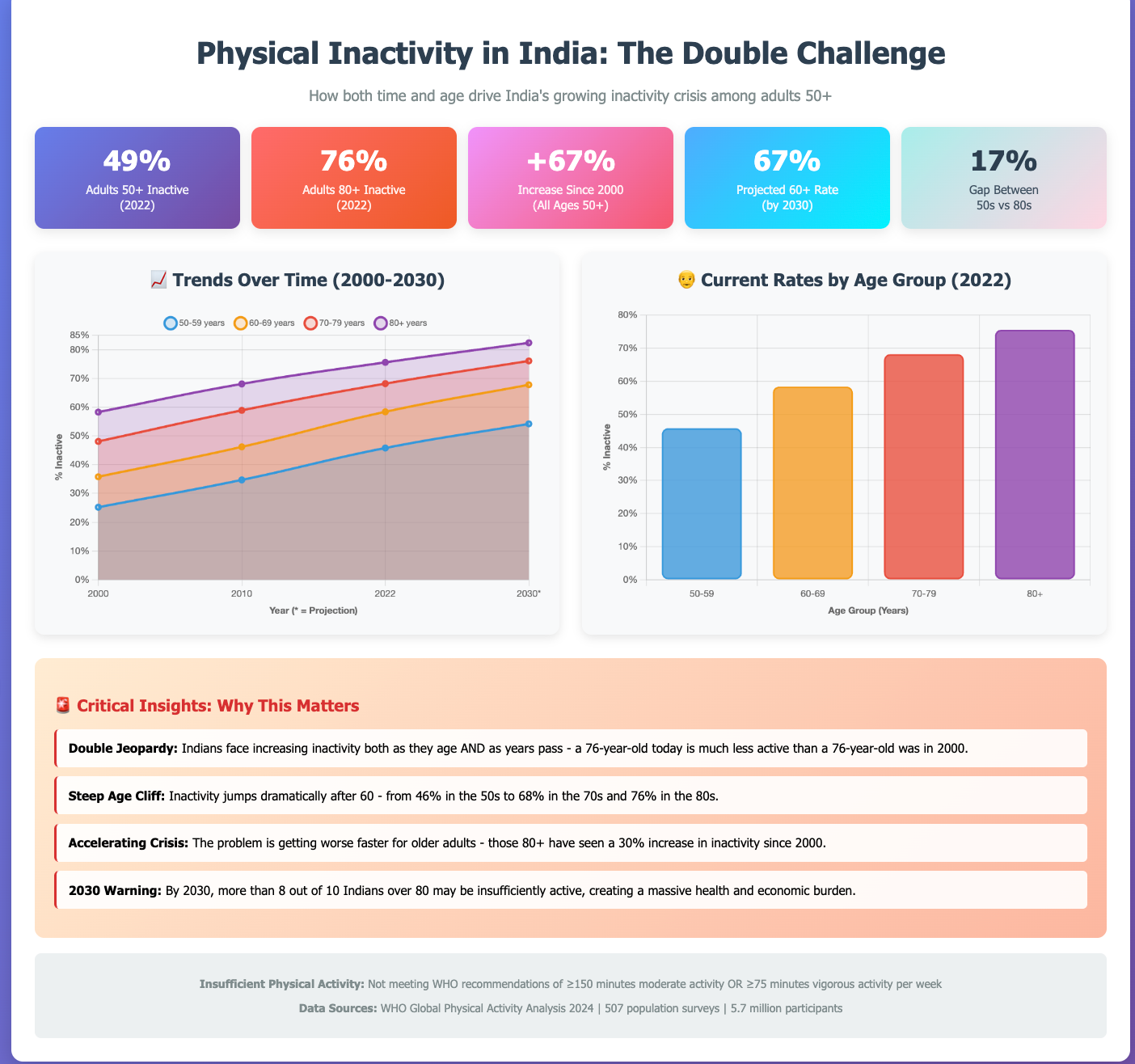
This shows that the older an Indian gets, the more inactive the person is…it is possible that the inactivity is a result of illness and inability to walk/run/exercise, but irrespective of the reason, the inactivity eventually kills…doesn’t matter what the cause and effect is.
Moreover, this data is based on self-reported surveys and just based on what I see daily, I would assume this to be gross underestimation.
This means that if you are unable to be fit to counteract the effects of being overweight, then perhaps it becomes necessary to address the overweight/obesity issue directly, something I didn’t write or talk about because the focus has always been only “moving” and not on “what happens if people don’t move”.
How do we know if someone is overweight/obese. Currently, all definitions are based on the BMI (body mass index), a ratio of weight over height. Just based on BMI, the Lancet data from 2024 [2] shows reasonably alarming trends in those over 50.
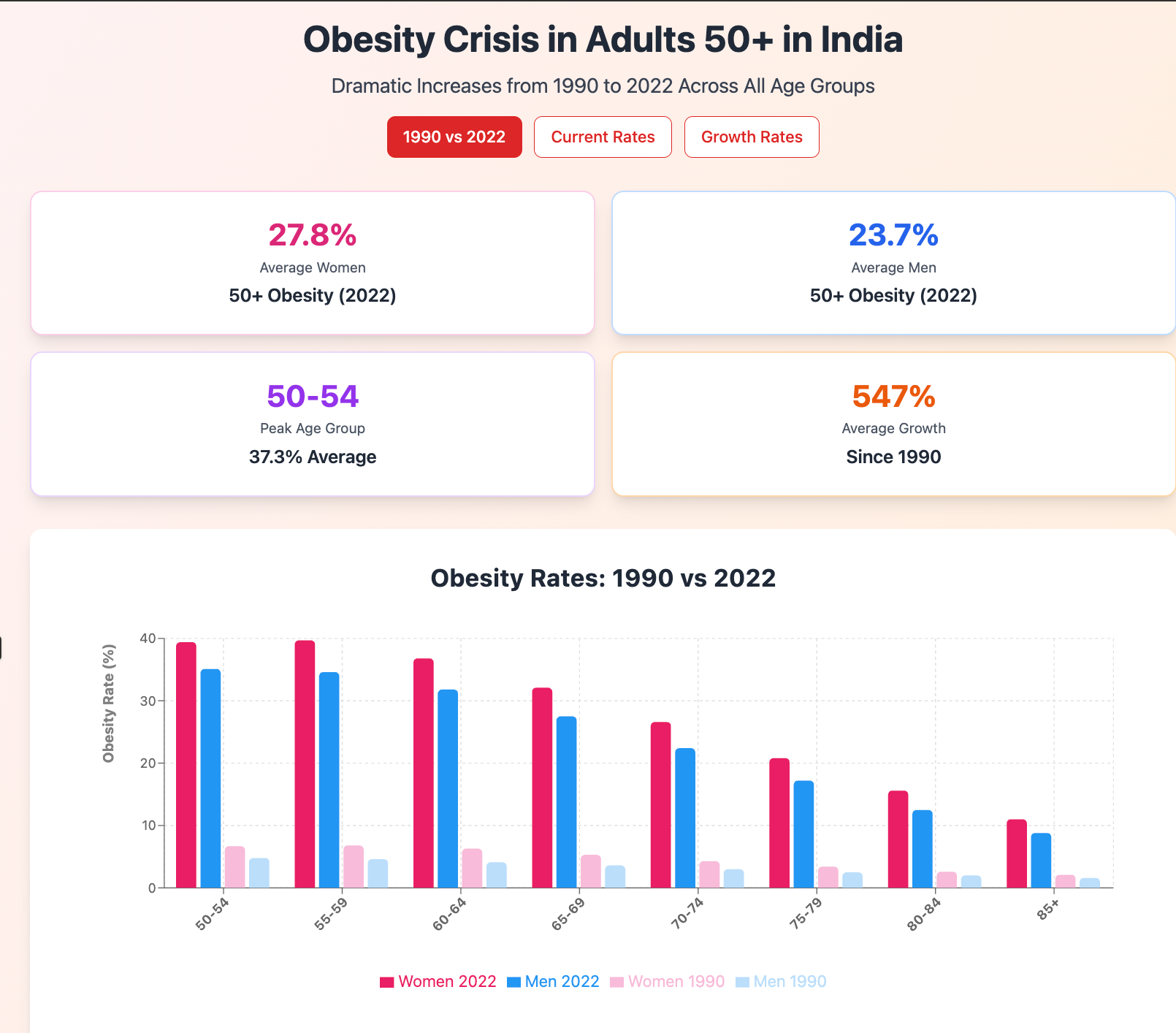
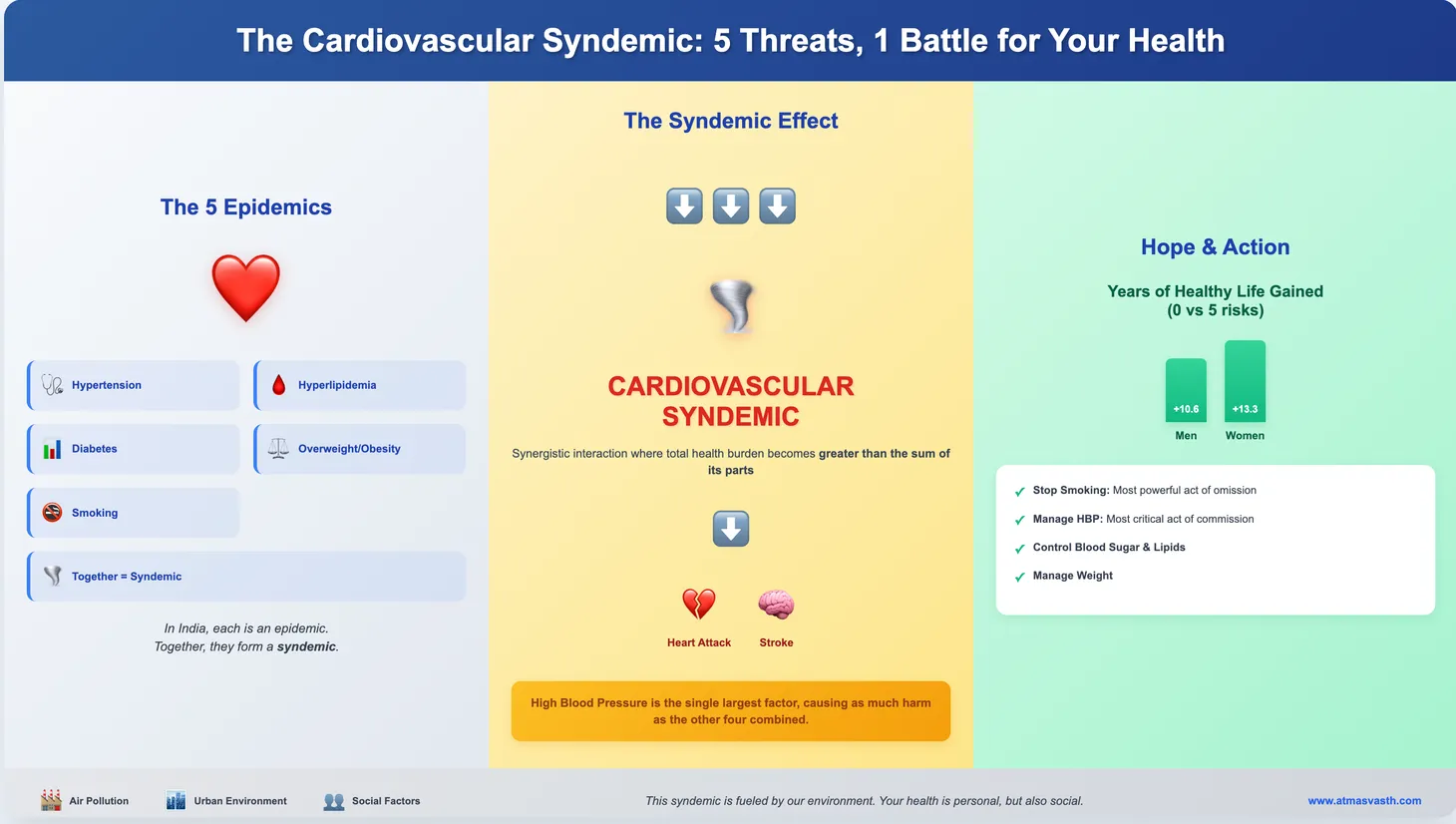
And if we superimpose the physical inactivity data, we can see that both are rising…physical inactivity and overweight/obesity in India.
BMI is a flawed concept due to a variety of reasons, but is used widely because it is easy to measure and has seeped deeply into our psyche. The American Medical Association (AMA) in 2023 made a public announcement to this effect saying that there are many other parameters that are perhaps more relevant and they named visceral fat, body adiposity index, body composition, relative fat mass and waist circumference.
Recently, a Lancet commission [3] got together to try and address these definitions better and they came up with “clinical obesity” and “preclinical obesity”. They defined obesity simply as “characterized by excessive adiposity, with or without abnormal distribution or function of the adipose tissue”. In short, expansion of adipose tissue in the body, if it causes disease is “clinical obesity” and if it doesn’t is “preclinical obesity”, different from merely being overweight as per BMI criteria. If therefore, an assessment of excess adiposity has to be made, then either anthropomorphic criteria (waist to height ratio, waist to hip ratio) or direct measurement of fat is needed.
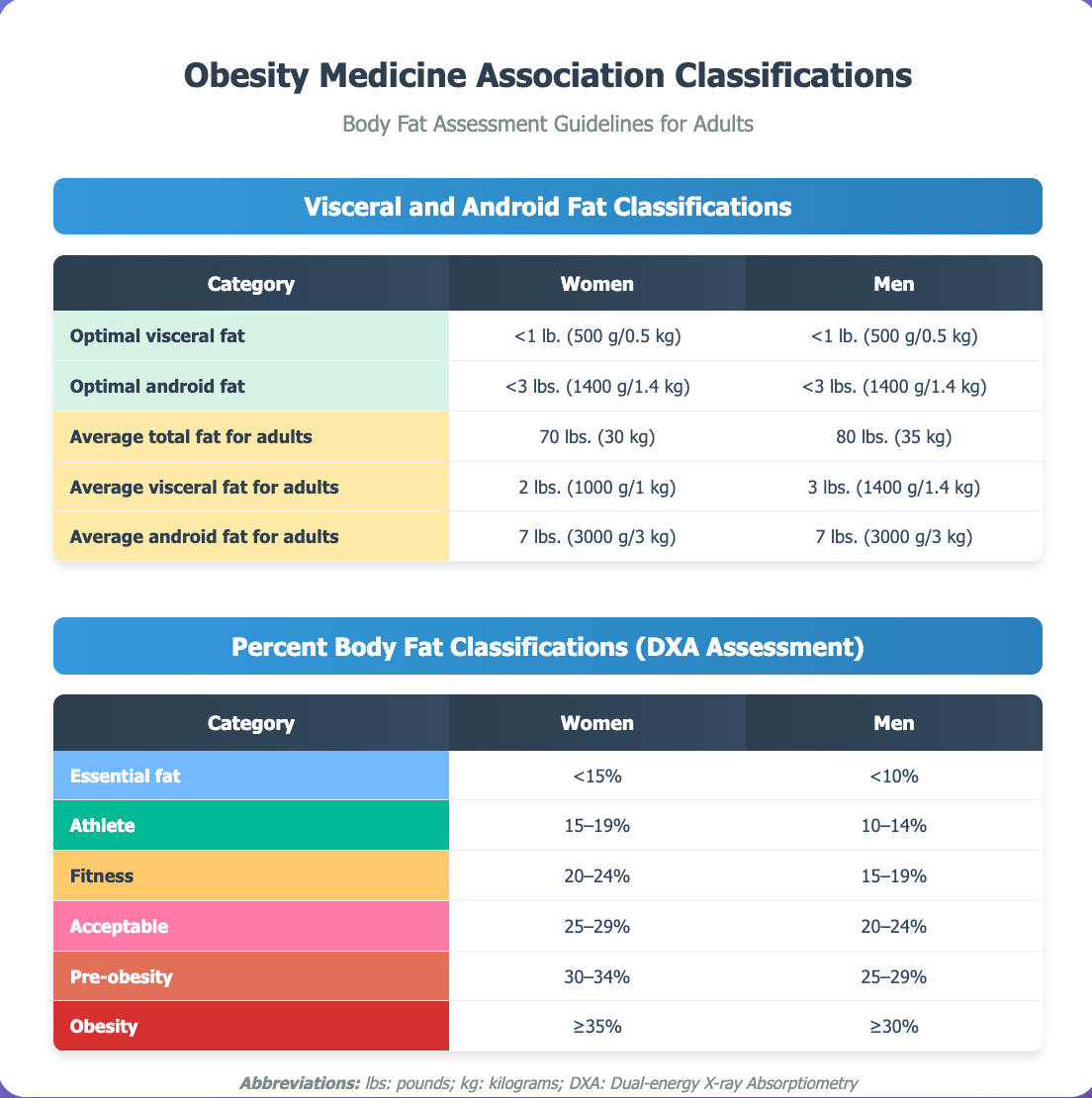
Direct measurement of fat is typically done by dual X-ray absorptiometry (DXA) or bioimpedance, though in the future both MRI and CT scans will give fat distribution and body composition results, as long as the study includes some abdominal scan…currently though, these are too expensive to use for fat distribution analysis.
I first mentioned DXA as a tool for screening for osteoporosis. DXA in the whole body mode also measures body composition and gives values of fat and lean mass in different parts of the body. More importantl,y it distinguishes “android” fat from “gynoid fat”, the android fat being the visceral body fat associated with adverse consequences [4].
In 2022, the Obesity Medicine Association (OMA) [5] came out with classifications based on the percent body fat measured using DXA scanners, along with optimal and average values of visceral and android fat for adults.
One of the challenges of weight loss programs is that while they may help with reducing overall weight, the interventions rarely if ever specifically target visceral/android fat and if that is really more important from a health perspective than just overall weight, then we need better interventions.
In my 1st June piece on the new GLP-1 agonists, Ozempic and Mounjaro, I talked about how these two drugs, semaglutide and tirzepatide respectively, are changing the obesity landscape, by providing effecting reduction of body weight and control of diabetes, among other benefits. In at least two of the trials, there was specific mention of reduction of visceral fat/visceral adipose tissue, measured using DXA [6].
David Kessler whose two pieces in The Atlantic and The New York Times, I quoted in that article focused on the reduction in visceral fat as a game changer with these drugs.
What does this mean for you and I?
1. BMI is a not a great method to assess risk from excessive or abnormal distribution of fat.
2. If you have an expanded waist, it is likely you have excess visceral fat.
3. If you are fit and active and illness free and not morbidly obese (BMI over 35 kg/sq m), then you may not need to do anything because your fitness offsets the adverse effects of excessive fat.
4. However, if you are unfit and/or don’t exercise, irrespective of what you do with food intake, which only leads to yo-yoing of weight, you may need to address your visceral fat increase. Either you can start becoming very fit, or you might have to start considering the use of GLP-1 agonists.
5. Also, if you are fit and active, but have diabetes or high blood pressure or elevated cardiovascular risk, you might still want to consider speaking to your doctor about the use of GLP-1 agonists, especially if your abnormal visceral fat situation does not change.
6. It may therefore be a good idea to measure your baseline visceral fat with a DXA study or ask for a body composition analysis, the next time you go for an osteoporosis screening study.
7. If you are anyway going to start taking GLP-1 agonists, either because you want to or because your doctors have asked you to, it may be a good idea to measure your visceral fat with DXA before starting, so you can track it over time.
In the future, as we have more data regarding visceral adiposity and the relationship of reduced android fat and improved healthspan and lifespan especially when used with GLP-1 agonists and whether tracking change with DXA or bioimpedance makes a difference, I will keep updating this site.
Footnotes
1. Strain T et al. National, regional, and global trends in insufficient physical activity among adults from 2000 to 2022: a pooled analysis of 507 population-based surveys with 5·7 million participants. The Lancet Global Health. 2024 Aug;12(8):e1232–43.
2. Phelps NH et al. Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. The Lancet. 2024 Mar;403(10431):1027–50.
3. Rubino F et al. Definition and diagnostic criteria of clinical obesity. The Lancet Diabetes & Endocrinology. 2025 Mar;13(3):221–62.
4. Sattar N et al. Tirzepatide and muscle composition changes in people with type 2 diabetes (SURPASS-3 MRI): a post-hoc analysis of a randomised, open-label, parallel-group, phase 3 trial. The Lancet Diabetes & Endocrinology. 2025 Jun;13(6):482–93.
5. Burridge K et al. Obesity history, physical exam, laboratory, body composition, and energy expenditure: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022. Obesity Pillars. 2022 Mar;1:100007.
6. Neeland IJ et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. The Lancet Diabetes & Endocrinology. 2019 Sep;7(9):715–25.
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.