Screening Mammography Saves Lives and Will Save Yours Too
Every woman between 40-75 years of age, who has the means, should get one screening mammogram done every year. Screening mammography saves lives and will save yours too
You can listen to the audio/podcast hosted on Soundcloud by clicking the Play button below within the browser itself.
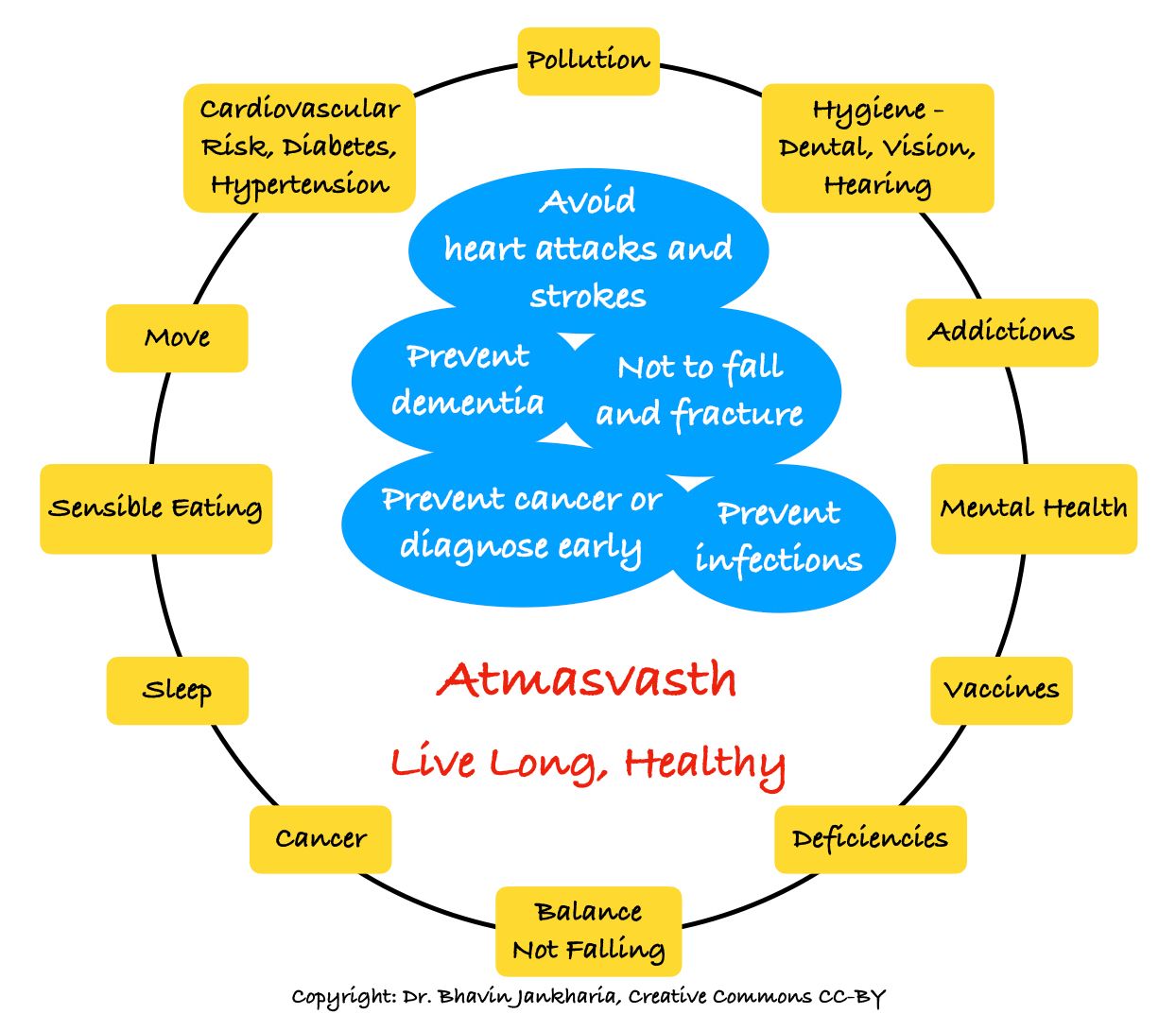
It is unfortunate that this message has been subverted at multiple levels for multiple reasons. The simple truth is “Screening mammography yearly between the ages of 40-79 picks up cancers early, ensures they get treated in time, reduces mortality and increases your lifespan.”
How good is the data?
Very good. Except for one Canadian study [1] in the 90s that did not show benefit and is the only one quoted by all the screening mammography nay-sayers, every other study [2] around the world, over the last three decades, has shown a positive benefit of screening mammography with respect to reducing mortality and improving longevity.
The latest is an elegant study out of Sweden [3], where they compared those who had done their last two screens (serial participants) with those who had done only the last but not the one previous (intermittent participants), done the last but one, but not the last (lapsed participants) and were never screened (serial nonparticipants). Serial participants had a 49% lower risk of death from breast cancer as compared to serial nonparticipants with the others falling in-between.
So what is this Canadian study?
It came out in the 90s [1] and did not find that screening mammography was beneficial. Like the “radiation causes cancer” argument the methodology was flawed [4], which has been pointed out multiple times, but those who are opposed to mammography use this one study to negate the benefits of screening mammography.
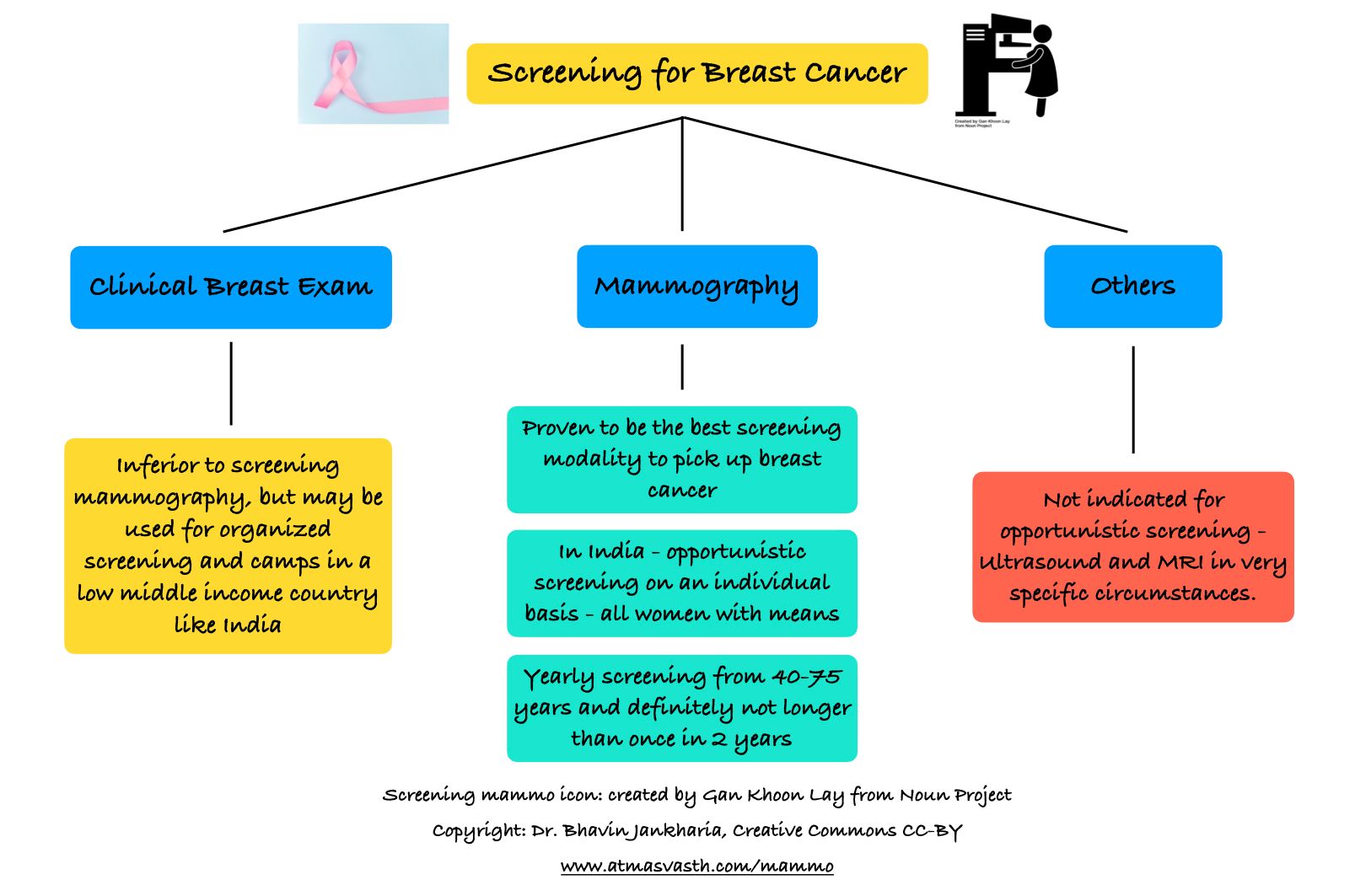
Why does Tata Memorial Hospital only advocate Clinical Breast Examination (CBE) [5]?
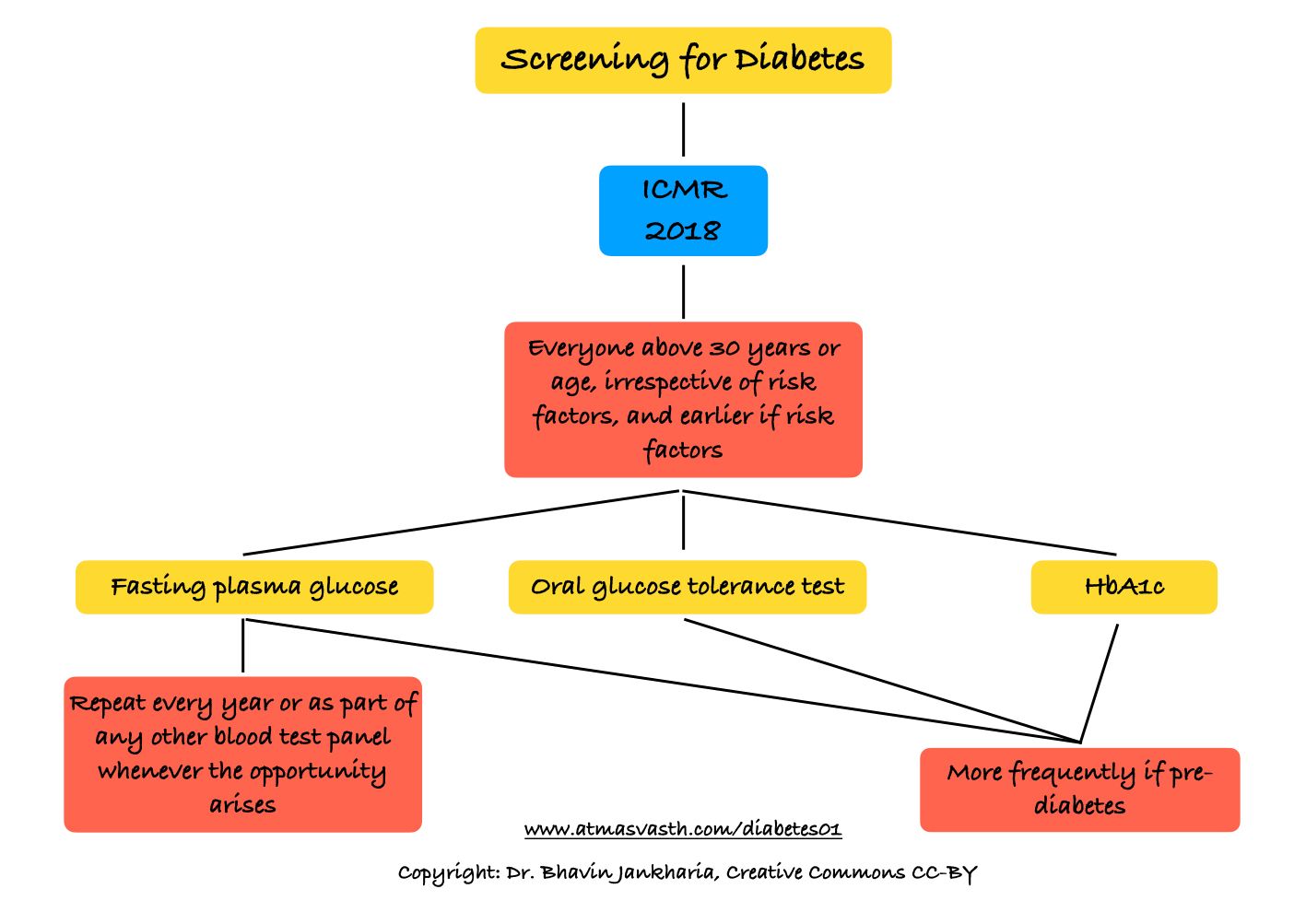
This brings us to the difference between population/organized screening and individual/opportunistic screening, which I discussed last Wednesday in the context of diabetes screening.
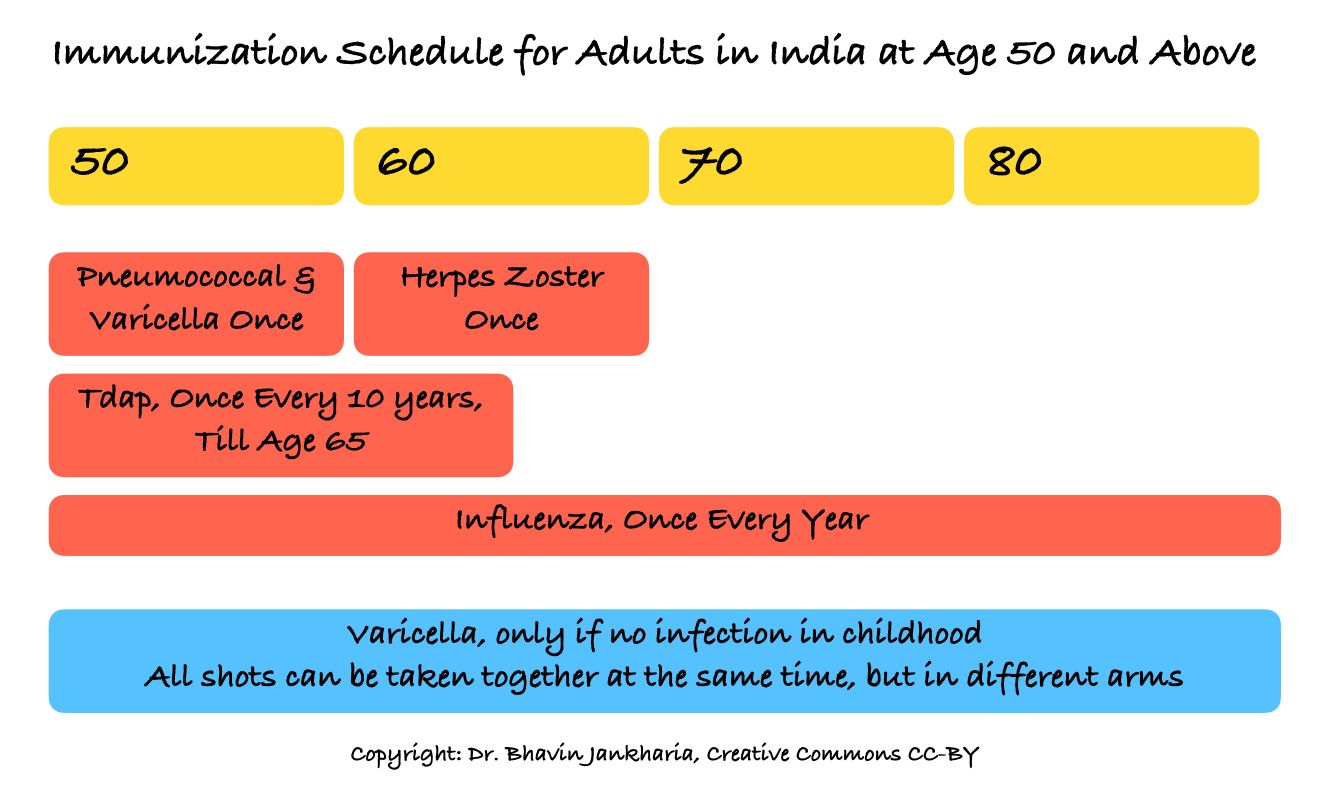
For population screening, a Government or health agency has to figure out the cost benefit ratio based on the resources that it has versus the net benefit the population would get, as was done in Austria, for example, for breast cancer, in 2014 [6]. The Indian government has no organized screening for any disease, to the best of my knowledge. Just to explain the difference a little better; all childhood vaccination in India is organized and free, while all adult vaccinations are opportunistic or left to the individual to take. Covid-19 vaccination efforts fall in between - it is an organized effort, but there is also an opportunistic component. But this is in the realms of disease prevention not diagnosis of disease by screening.
As I discussed on Wednesday with respect to diabetes screening, when the USPSTF reduced the age for screening for diabetes to 35 years, it made free screening accessible to a larger population…the tab for the screening is picked up by insurance or the health authorities in countries like the US.
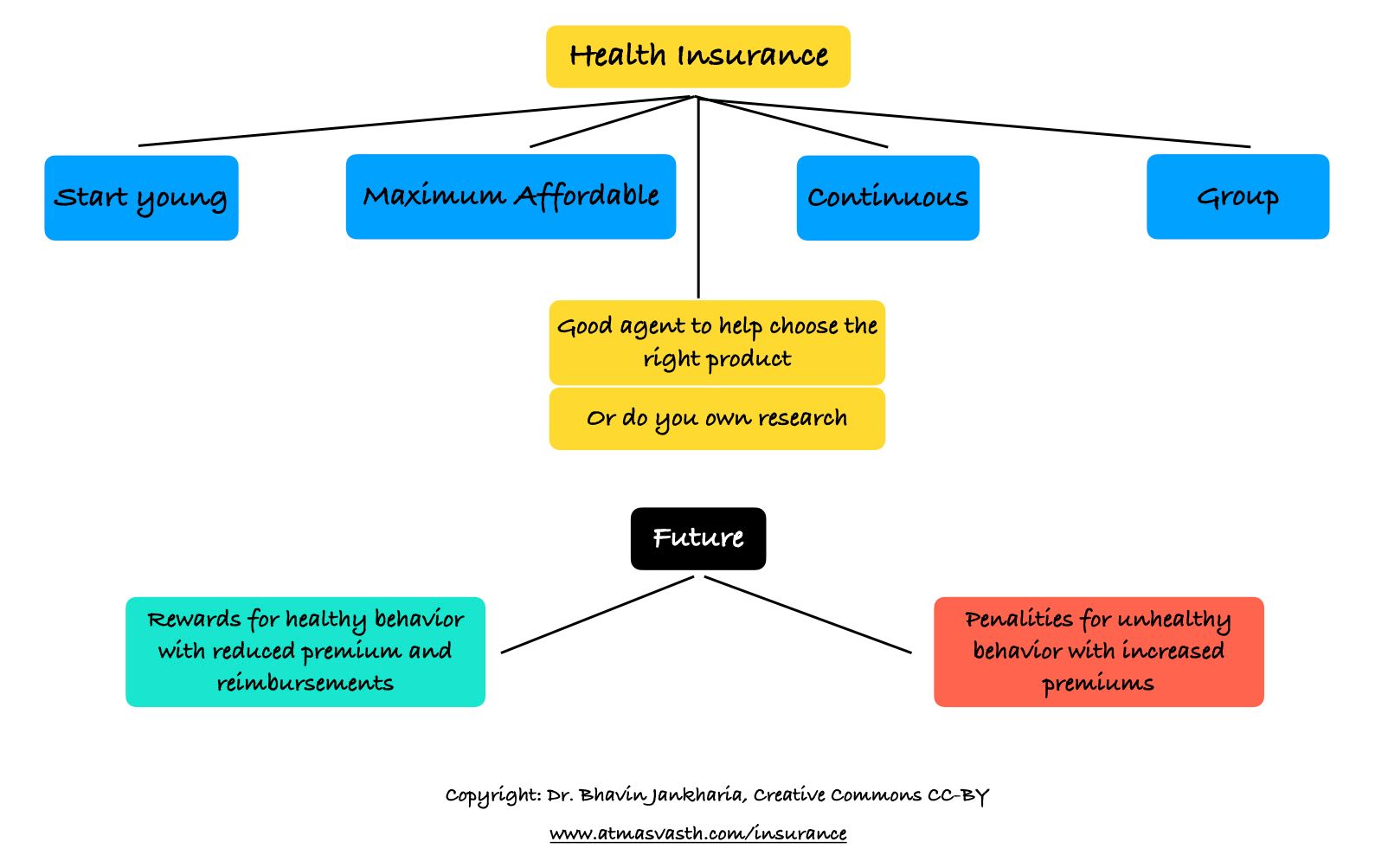
Similarly, screening mammography is offered for free by insurance and Govt authorities in the US, though the guidelines vary, depending on the organization, such as the USPSTF or American Cancer Society or the American College of Radiology, ranging from once a year to once in two years for different age groups. In the UK, any British national between the ages of 50-71 can get a free screening mammogram done in any National Health Service Hospital, once in 3 years, but if you want to pay and get one one done every year, no one will stop you.
India cannot afford organized screening to be paid for by the Government, when it can’t even offer free fasting plasma glucose tests to our population to try and diagnose diabetes, which currently affects 11.7% of the adult population, while the prevalence of breast cancer currently is estimated to be 914,644 women [7,8], which is close to 10 lakhs or 1 million, which is prevalence percentage of 0.6% of women above the age of 50 years (150 million or 15 crores). For more data and numbers, please see the Footnote.
So there is no way that the Govt can afford to provide mammography services for a disease that affects only 0.6% of the above 50-years female population. But breast cancer is the most common cancer in women in India [8], with a rising incidence (partly because women are living longer and partly because of improved detection), and the commonest cause of cancer death in women.
Tata Memorial Hospital launched a big study on Clinical Breast Examination, almost 20 years ago, which showed that CBE saves lives and reduces mortality, compared to not examining the breast at all. Obviously. For a country like India, anything is better than nothing and hence CBE by health workers like ASHA workers, would go a long way in picking up breast cancer, especially in areas where health services are poor. What the TMH study and press releases did not mention is that for a low middle income country like India, CBE would be a good method for organized screening if the Govt or other health authorities did decide to offer it, but it is inferior to screening mammography for opportunistic screening, if a woman with resources wants to do it herself or a hospital or community with means wants to promote it.
While the Govt cannot afford to subsidize or offer screening mammography to everyone eligible in the country (which would be around 150-200 million women and we have at best around 300-400 mammography units in the country - you can do the math), every Indian woman who has the means and resources to get herself screened should do this at a good centre every year and definitely not at a longer interval than once every two years. The Breast Imaging Society of India (BISI) also advocates annual screening with mammography, despite the lack of Indian data.
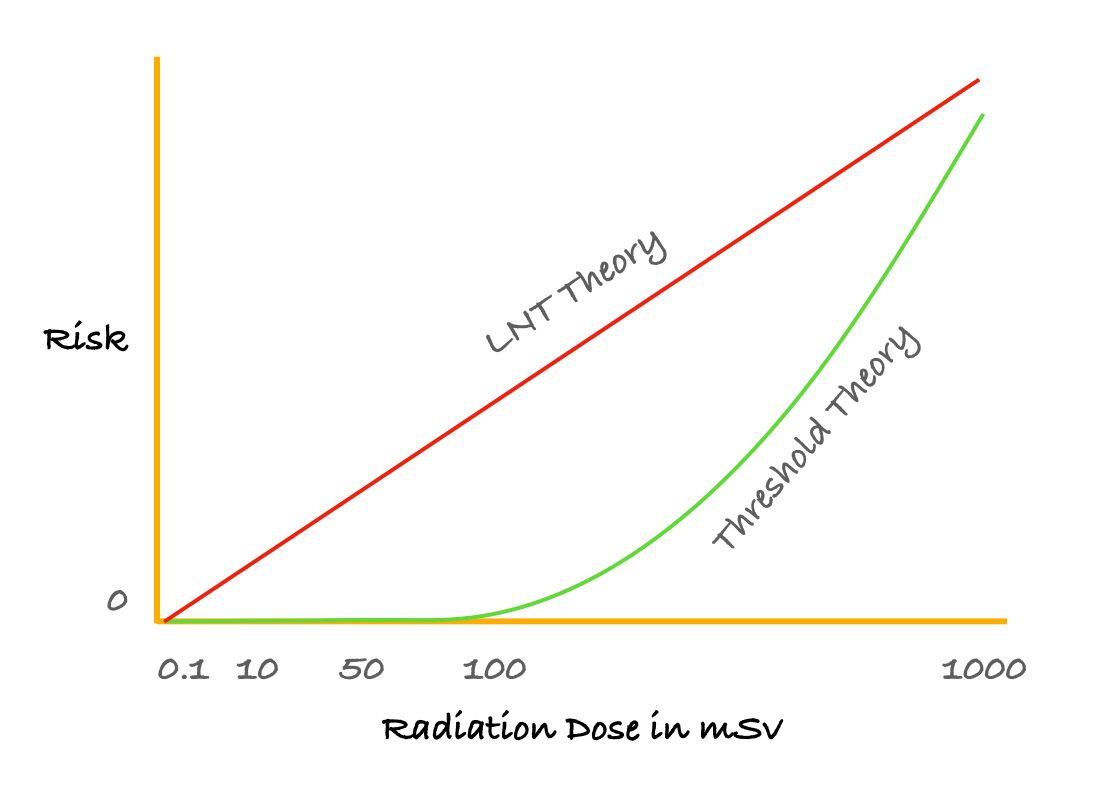
But doesn’t screening mammography involve radiation and cause cancers of the thyroid and breast?
I addressed this a few months ago when I spoke about radiation from CT scans of the chest. Mammography involves even lesser radiation and given that there is no evidence that radiation from any diagnostic imaging test causes cancer, there is no radiation risk from mammography.
The “radiation from mammography causes thyroid cancer” is a meme that started with Dr. Oz and is completely illogical.
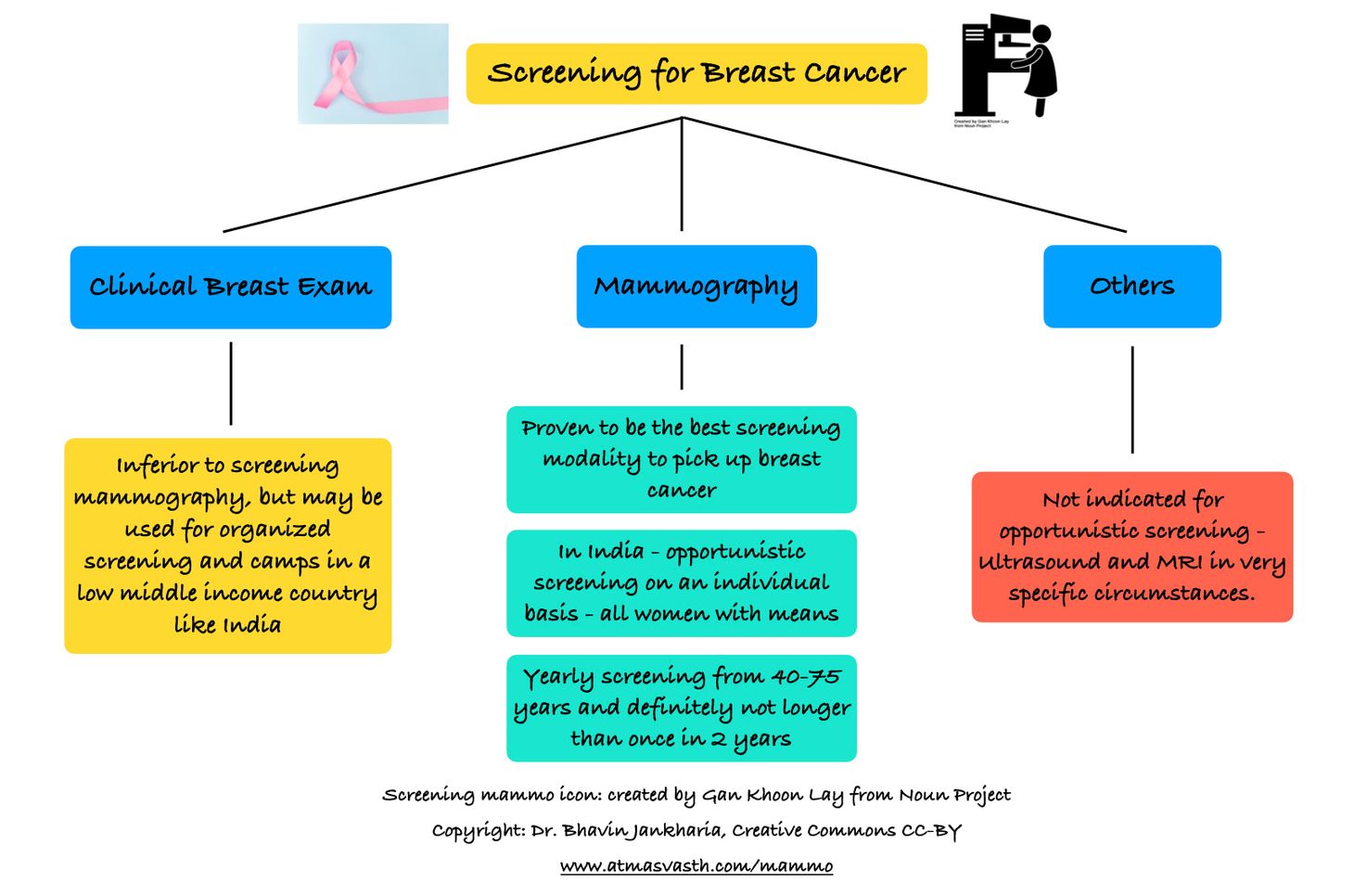
What about alternative techniques like ultrasound for screening or thermal screening offered by private companies?
Ultrasound for screening is inferior to mammography except in young women below the age of 30 years who have dense breasts, where mammography may miss lesions. That is the only time to do ultrasound screening.
Thermal scanning and similar technologies are unproven. Obviously if there is a lump, it may be picked up, just like CBE may pick these up. Only in India, with lax regulations, can you offer services like thermal scanning for breast cancer screening without proof or any large scale data and get away with doing anything you want to do. At best, they may be useful for population screening if they are cheaper than screening mammography.
To repeat, CBE, ultrasound and mammography are the only techniques where a large number of large scale studies have shown they work and of these, screening mammography is the study of choice.
What about MRI for screening?
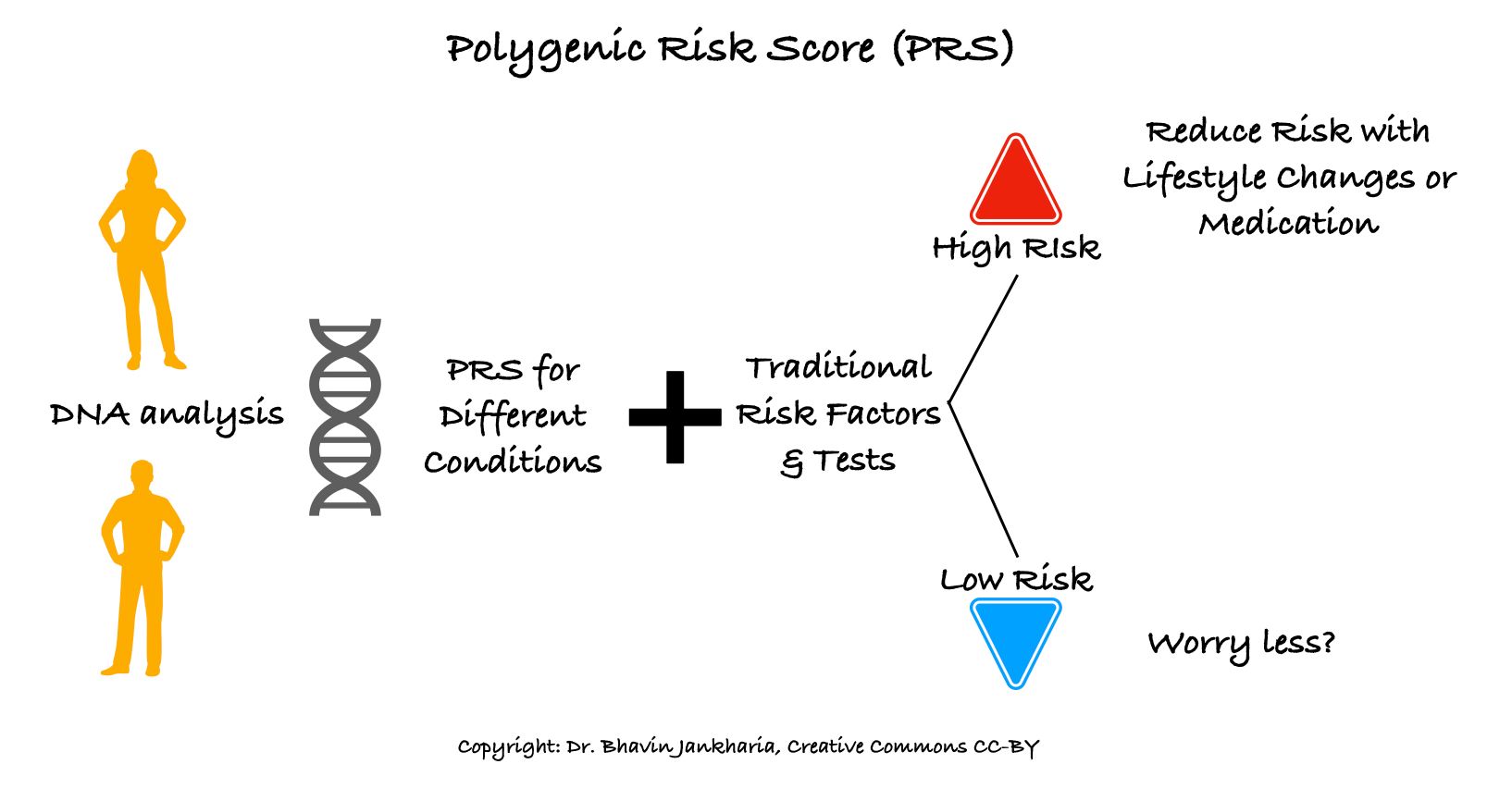
This is done only in specific high risk individuals, in those who typically have a genetic predisposition like my friend with BRCA1 and BRCA2 genes, who I had mentioned earlier. The doctors will decide if this is necessary.
Isn’t screening mammography painful because of the breast compression?
Yes it can be. Some technicians are better than others, but you can still get pain and sometimes with the same technologist, you may get pain one year and not get pain another year. It is momentary, and is worth bearing for the long-term benefit the test offers.
Where should I get screening mammography done?
With any reputed centre or hospital that has trained mammography radiologists and technologists. More importantly, ideally, serial mammograms should be repeated at the same place, so that the same people are able to compare and see if anything has changed. If the screening mammogram is done using full-field digital methods including a new technique called digital tomosynthesis, then the repeat scan should also be at the same place to allow side by side comparison on the workstation.
So, if you are a woman between the ages of 40-75, or have a mother, sister, daughter or any female relative in this age group, please ensure you or they get one screening mammogram per year and if there is a logistics issue, then at an interval not longer than once in 2 years, preferably at the same imaging centre or hospital.
Last Wednesday's Post
Last Sunday's Post
Posts Referenced in this Piece
Essential Reading
Please see the Archives for the rest of the posts.
Footnotes
Data on prevalence and incidence
The incidence of breast cancer is approximately 0.13% of the population of women at risk above the of 50 years (205,538 divided by 150 million women) as of 2021 projected, up from 118,000 in 2016 [7]. The prevalence in 2016 (i.e. the total number of women with breast cancer alive in 2016 was 526,000 [8], a factor of 4.45 times the yearly incidence, which in 2021 works out to a prevalence of 914,644 or close to a million (10 lakh) women, which is a prevalence percentage of 0.6% of women above the age of 50 years.
1. Miller AB, Baines CJ, To 7, Wall C. Canadian National Breast Screening Study. 1 . Breast cancer detection and death rates among women aged 40-49. Can MedAssocJi992:147:1459-1476
2. Feig SA. Influence of Patient Participation on Decreased Mortality from Screening Mammography. Radiology. 2021 Jun;299(3):548-549. doi: 10.1148/radiol.2021210226. Epub 2021 Mar 30. PMID: 33788587.
3. Duffy SW, Tabár L, Yen AM, et al. Beneficial Effect of Consecutive Screening Mammography Examinations on Mortality from Breast Cancer: A Prospective Study. Radiology. 2021 Jun;299(3):541-547. doi: 10.1148/radiol.2021203935. Epub 2021 Mar 2. PMID: 33650900.
4. Kopans DB, Feig SA. The Canadian National Breast Screening Study: a critical review. AJR Am J Roentgenol 1993;161(4):755–760.
5. Mittra I, Mishra GA, Dikshit RP et al. Effect of screening by clinical breast examination on breast cancer incidence and mortality after 20 years: prospective, cluster randomised controlled trial in Mumbai. BMJ. 2021 Feb 24;372:n256. doi: 10.1136/bmj.n256. Erratum in: BMJ. 2021 Mar 19;372:n738. PMID: 33627312; PMCID: PMC7903383.
6. Schiller-Fruehwirth I, Jahn B, Einzinger P, Zauner G, Urach C, Siebert U. The Long-Term Effectiveness and Cost Effectiveness of Organized versus Opportunistic Screening for Breast Cancer in Austria. Value Health. 2017 Sep;20(8):1048-1057. doi: 10.1016/j.jval.2017.04.009. Epub 2017 May 16. PMID: 28964436.
7. D'Souza ND, Murthy NS, Aras RY. Projection of cancer incident cases for India -till 2026. Asian Pac J Cancer Prev. 2013;14(7):4379-86. PMID: 23992007.
8. India State-Level Disease Burden Initiative Cancer Collaborators. The burden of cancers and their variations across the states of India: the Global Burden of Disease Study 1990-2016. Lancet Oncol. 2018 Oct;19(10):1289-1306. doi: 10.1016/S1470-2045(18)30447-9. Epub 2018 Sep 12. Erratum in: Lancet Oncol. 2018 Oct 3;: PMID: 30219626; PMCID: PMC6167407.
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.