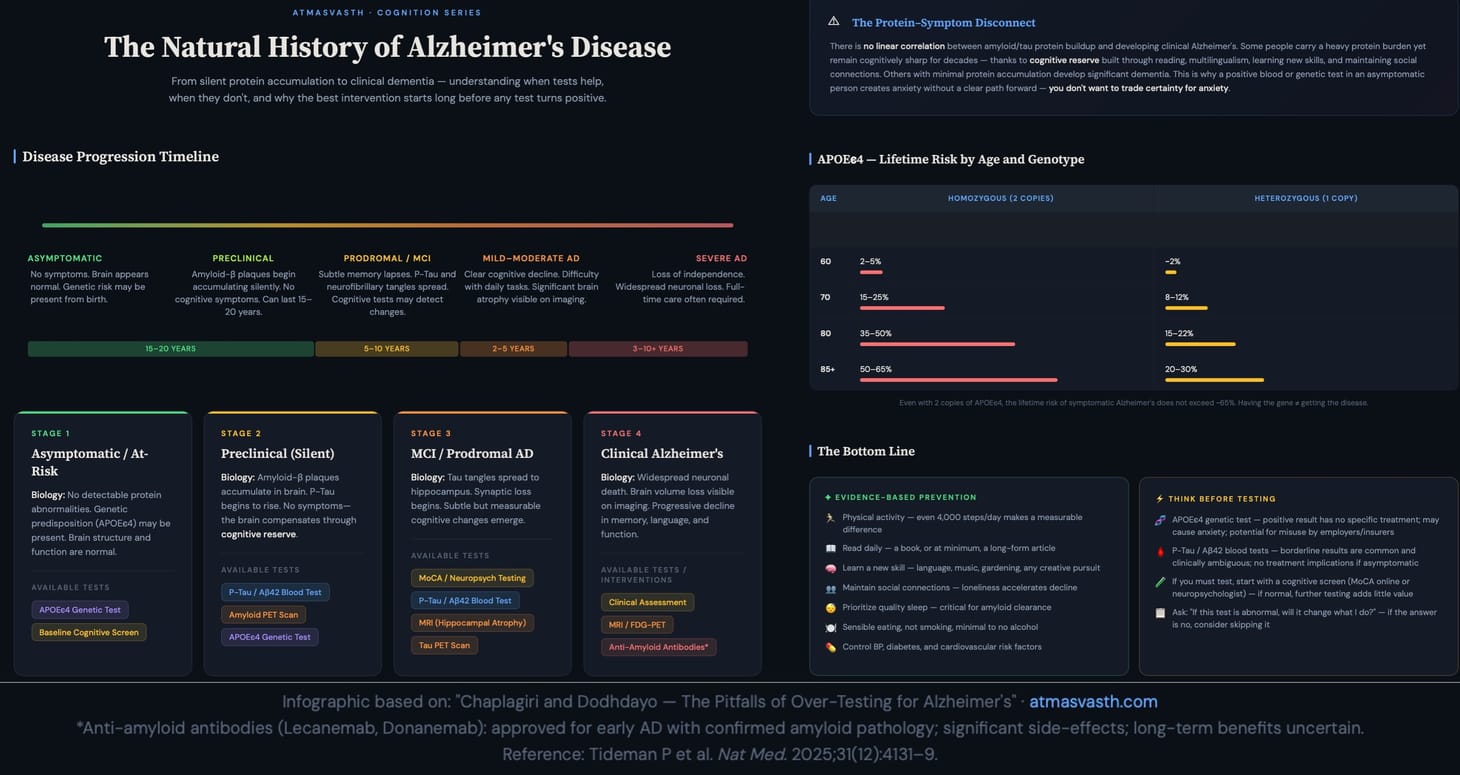
Chaplo and Dodhdayo...The Pitfalls of Over-Testing for Alzheimer's
Just because you can test, doesn't mean you have to
The Book
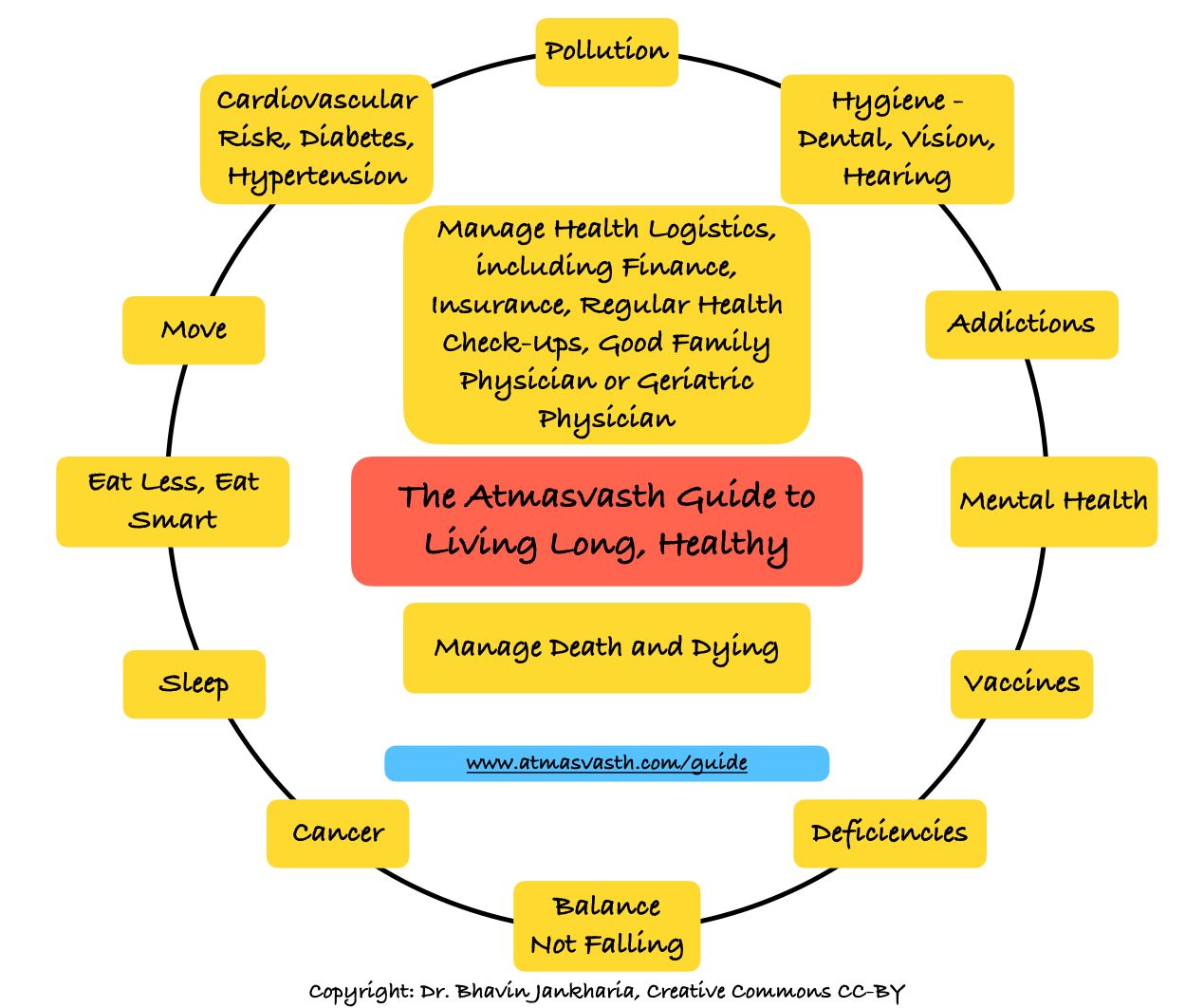
The Detailed 15-Point Guide to Live Long, Healthy
Audio
Soundcloud
YouTube
A YouTube version of the audio is also now available here.
Text
We don’t want heart attacks, strokes, cancers and bad infections. We don’t want to fall, fracture, be frail or have sarcopenic muscle weakness. We don’t want dementia.
Of all these issues that define the end-goals of our atmasvasth quest to live long, healthy, to me, the most important is “not losing it”. I don’t want to be cognitively impaired, I don’t want to get dementia and I don’t want to be dependent on others for my daily needs.
In the 15-point guide, the 4th point is
Prevent/delay cognitive decline/dementia
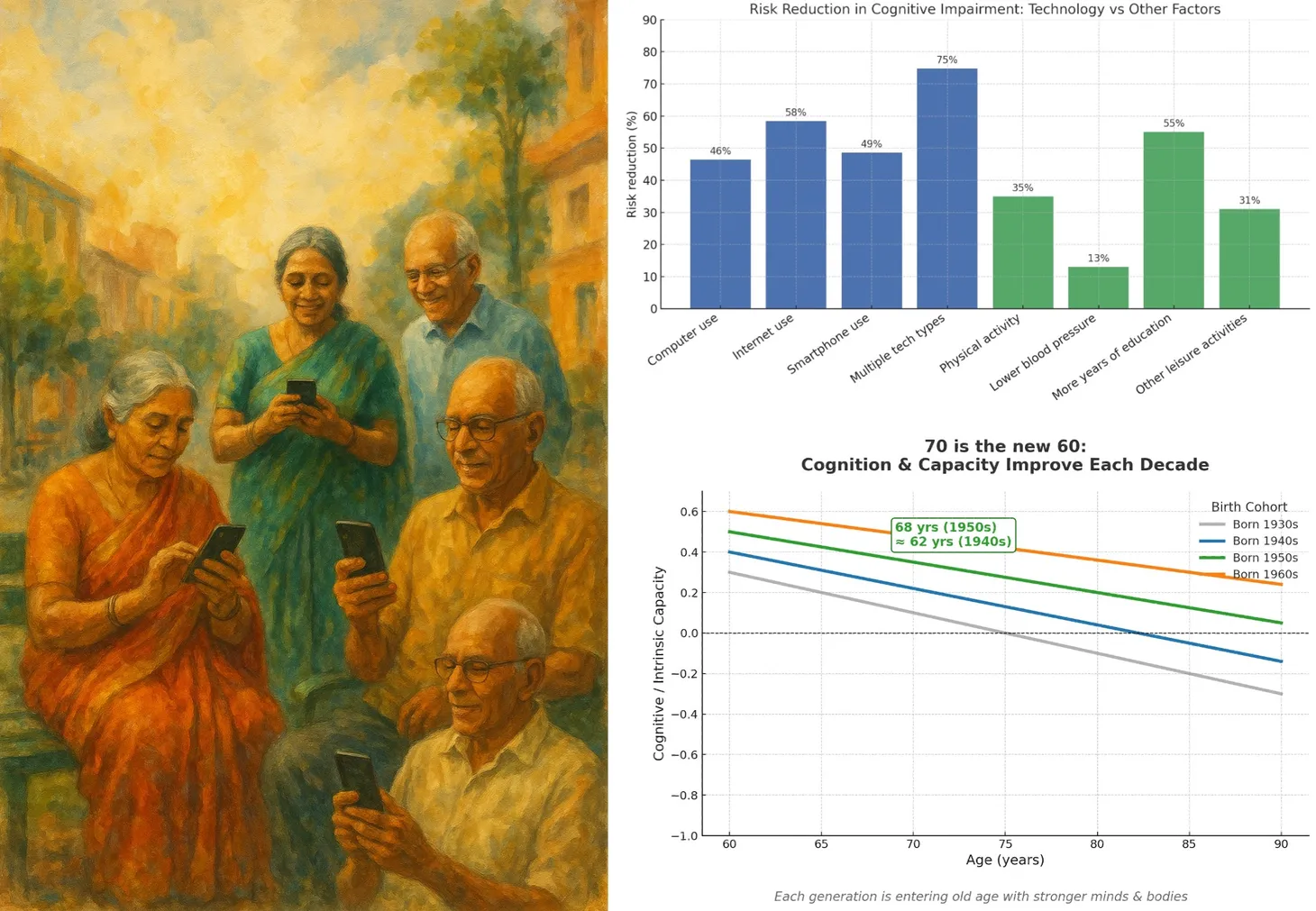
- Physical activity, good sleep, sensible eating, not smoking and minimal to no alcohol - help reduce cognitive decline. Specifically, 4000 steps a day make a difference.
- Read - preferably a book, else a long article, daily.
- Learn a new skill - language, musical instrument, singing, dancing, gardening, any creative experience makes a difference.
- Maintain social connections - to prevent loneliness, which can accelerate cognitive decline.
- Being multilingual builds cognitive reserves.
- In the future, if robust drugs become available to prevent/treat cognitive decline, then genetic and blood testing will also become routine.
In my July 2024 piece titled Cognition and Dementia Updates, this is what I ended with.
What does this mean for you and I?
Genetic or blood testing for MCI or AD may be premature if you have no signs or symptoms of cognitive impairment because there isn’t much you can do with a positive test. If you want to test though, the current standard of care is a standard cognition test (language, memory, etc.) with a neuropsychologist. However, this may change as the field progresses and I will keep you updated.
Preventing MCI and AD is based on lifestyle factors (sensible eating, physical activity, adequate sleep, not smoking), controlling high blood pressure, diabetes, reducing cardiovascular risk (statins, aspirin, if indicated), and maintaining social connections and increasing cognitive reserve by reading and engaging in activities that stimulate the mind.
In the future, there may be treatment options available for MCI and AD, and I’ll write about them as they emerge.
This is a rapidly moving field, so let’s fast forward to Feb 2026.
It would be logical to assume that any test that helps determine risk is useful and gives a sense of what to do and what to expect.
One risk factor for Alzheimer’s is the APOEϵ4 gene. If you have two copies, it is highly likely you will develop the underlying brain changes (amyloid and tau) if you live long enough, but the absolute lifetime risk of symptoms will be around 50-65% and if you have one allele, 20-30%. This is because there is no linear correlation between the amount of abnormal protein buildup in the brain and developing signs and symptoms of Alzheimer’s disease. You may have a lot of abnormal protein accumulation and never get symptomatic Alzheimer’s or have minimal abnormal protein and still get bad dementia. The brain is remarkably resilient; some people can carry a heavy 'protein burden' but continue to remain sharp because of a high cognitive reserve. The risk is also age-based. At age 60, a homozygote (both alleles) would have an absolute risk of 2-5%, which then increases over time to reach 50-65% in those over 85 years of age.
I did get my genetic test done for APOEϵ4 and I don’t have this allele. But let’s say I did. What would that have meant, except for me to start worrying that each time I forget something, it might be Alzheimer’s and not something that just naturally happens?
And what do you do if you test positive? There is no treatment, except being physically active, getting enough sleep and eating sensibly and the rest of the points that are in the 15-point guide. Unless you actually have cognitive decline, the antibody treatment is not indicated and even then the cost-benefit ratio is not clear, given the significant side-effects and no one knows the long-term benefits of these treatments anyway.
There are also new blood tests [1] that measure the P-Tau and B-amyloid 1-42 levels in the brain. The higher the p-tau/b-amyloid ratio the more the chance of getting clinical Alzheimer’s dementia, though there is no clear correlation between the protein accumulation in the brain and actually getting dementia as I mentioned earlier.
I measured my levels last month at the only hospital that does it in, in Mahim, but I assume that all the major labs will soon be doing these tests.
The result was the worst. Neither low, nor high…borderline. Which means…and I am back to where I started.
Even if the value was high, what would that have meant? Was I going to do anything different? Would I have started working out more, running more, changing my food habits even more, given that since the start of Atmasvasth in 2020, I have evolved along with my writings and follow most of the 15 points in the guide?
Merely having high risk does not imply that you will get the disease and if there is no specific treatment, then why bother?
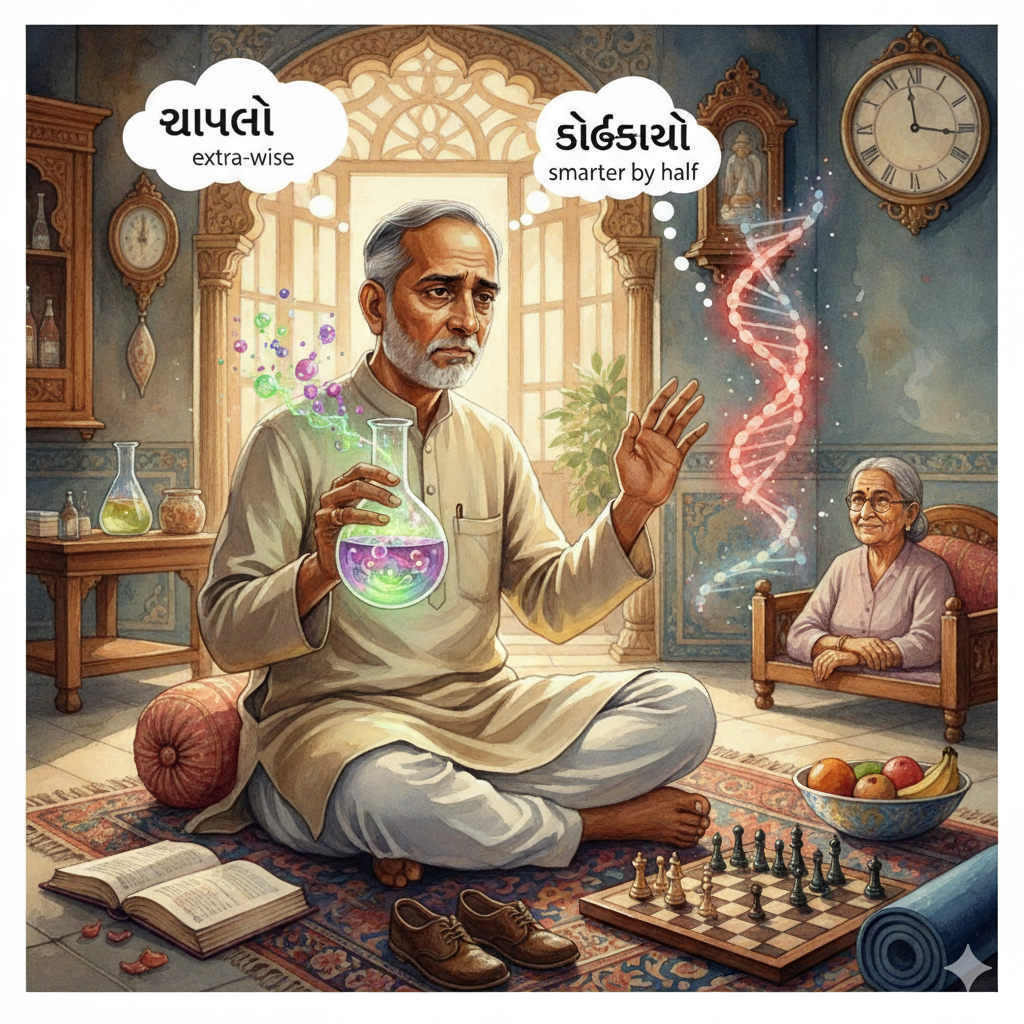
When I told my wife, she had only word…”chaplo”, which translates to being extra-wise and not in a good way. “Dodhdayo” is another Gujarati word that means “trying to be smarter by half and doing or saying unnecessary things that may often backfire”.
I anyway then did my cognitive testing online at https://mocacognition.com/digitaltools/ and at cognitivetest.me, though the latter charged me 20 odd US dollars for the report and the results were good which means that at least at this point I do not have cognitive decline. Perhaps I should have started with this test and if it showed cognitive loss, then moved onto other tests.
We measure our blood pressure, because high blood pressure is a known risk factor for cardiovascular disease and lowering blood pressure with medications, reduces the risk of disease. We measure blood sugar and lipid levels for the same reasons. Screening tests where the outcomes have specific management tools.
I will never do my serum PSA, because the outcomes are messed up. If it comes high and an asymptomatic prostatic malignancy is found, which perhaps may have never grown or created problems, but is just one of those incidental cancers that over 30% of people over the age of 70 and almost 60-70% of men over 80 are found to have on post-mortem examinations, then all the treatment options have complications that are not worth the effort.
Every time you do a test for screening for disease, you must ask yourself, what the end point is, especially if the result is abnormal. If there is no treatment and if knowledge of that disease makes no difference otherwise, then the test is best avoided. We will discuss this again and again, soon in a post on “Surveillance Medicine” and another one later on the new cancer detection blood tests.

Let me give you an example though of surveillance medicine. Let’s say you do the APOEϵ4 test and you are found to have both copies and you are say 50 years old and your employer or insurance company gets hold of this. Your employer may not promote you, or may make life difficult for you in the company in an attempt to force you to leave the company so that they are not saddled with a potential liability in the future, or the insurance company might increase your premiums. Or the Govt may mandate you participate in a trial depending on the country you are in, even if you don’t want to.
So what does this mean for you and me?
Perhaps the simplest thing to is to follow the 15-point guide and do all the things that help with preventing cognitive decline, given that there are so many modifiable risk factors that can be controlled.
If you still want to know, then perhaps a test for cognitive decline (which you can test online at the sites I have mentioned or with a neuropsychologist) would help. However, if you test positive, it is likely that you truly have mild to moderate cognitive decline and would then need further disease assessment.
The challenge is if you are asymptomatic and/or test normal on the cognitive tests. Should you do genetic and blood testing for Alzheimer’s just to know what your possible potential risk is of developing Alzheimer’s as you age? Is it worth knowing this if there is no treatment at this stage? These are questions you have to answer for yourself and then decide with the understanding that even if you test positive, you may still never land up with dementia. You don’t want to trade certainty for anxiety.
Footnotes
1. Tideman P, Karlsson L, Strandberg O, Calling S, Smith R, Midlöv P, et al. Primary care detection of Alzheimer’s disease using a self-administered digital cognitive test and blood biomarkers. Nat Med. 2025 Dec;31(12):4131–9. doi:10.1038/s41591-025-03965-4
Atmasvasth Newsletter
Join the newsletter to receive the latest updates in your inbox.